 Dragon Teeth
Dragon Teeth Jurassic Park
Jurassic Park Micro
Micro The Great Train Robbery
The Great Train Robbery The Andromeda Strain
The Andromeda Strain The Lost World
The Lost World Congo
Congo Travels
Travels Timeline
Timeline Sphere
Sphere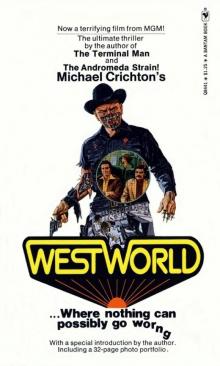 Westworld
Westworld Prey
Prey State Of Fear
State Of Fear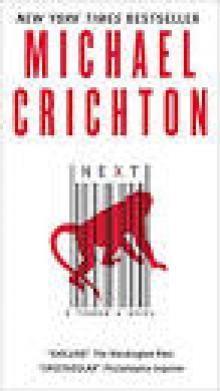 Next
Next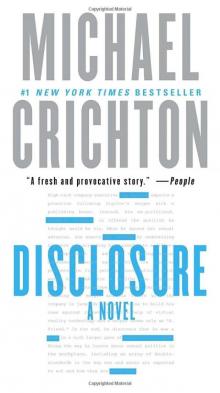 Disclosure
Disclosure Pirate Latitudes
Pirate Latitudes The Terminal Man
The Terminal Man Five Patients
Five Patients Rising Sun
Rising Sun Binary
Binary The Andromeda Evolution
The Andromeda Evolution Airframe
Airframe Easy Go
Easy Go Drug of Choice
Drug of Choice Odds On: A Novel
Odds On: A Novel Scratch One
Scratch One Dealing or The Berkeley-to-Boston Forty-Brick Lost-Bag Blues
Dealing or The Berkeley-to-Boston Forty-Brick Lost-Bag Blues Venom Business
Venom Business Grave Descend
Grave Descend Gold - Pirate Latitudes
Gold - Pirate Latitudes Binary: A Novel
Binary: A Novel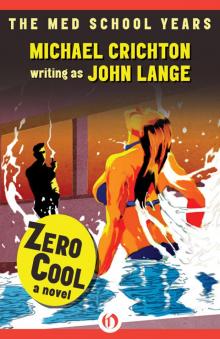 Zero Cool
Zero Cool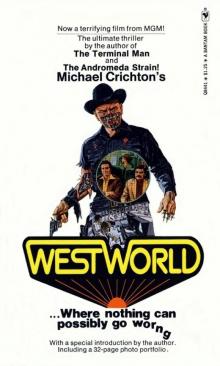 Delos 1 - Westworld
Delos 1 - Westworld